NG Vascular announces non-surgical option for chronic hemorrhoids
Hemorrhoidal artery embolization provides effective relief without the long, painful recovery associated with hemorrhoidectomy or banding
HAE carries a lower risk of bleeding, infections and other complications compared to surgery.”
MERRILLVILLE, IN, UNITED STATES, January 13, 2026 /EINPresswire.com/ -- A new therapy is now available for those suffering from chronic grade 1-3 internal hemorrhoids. Hemorrhoidal artery embolization (HAE) is an FDA-approved and clinically proven outpatient procedure that does not require any cutting or stitches within the anus or rectum.— Dr. Nazar Golewale
More than half of all Americans will experience hemorrhoids in their lifetime. Hemorrhoids are actually swollen veins, similar in nature to varicose veins. Most go away on their own with diet changes, topical treatments, medications or supplements. But for some they can persist for several months or longer, causing bleeding, itching and painful bowel movements.
A surgical procedure known as hemorrhoidectomy was historically used to treat chronic hemorrhoids. However, recovery is more difficult than other types of surgery because regular bowel movements put pressure on the surgical site, causing pain. Although effective, the surgery is associated with intense postoperative pain and a prolonged time to return to normal activities.(1,2) More recently a less invasive treatment called rubber band ligation (banding) became available. Unfortunately, this approach is also associated with pain and complications, especially for those taking anti-platelet or anti-coagulant medication, who have a higher risk of hemorrhage and infection.(3)
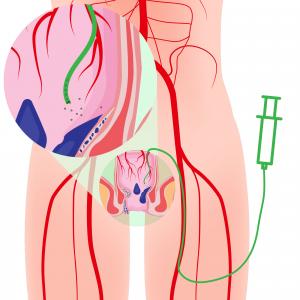
On the other hand, the HAE procedure is performed entirely within the body’s vascular system. An interventional radiologist uses imaging to guide a catheter from a tiny entry site in the wrist or thigh to the hemorrhoid. Special coils and/or sclerosing agents are then injected to cut off the blood supply to the hemorrhoid, causing it to shrink and symptoms to abate. It is safe and effective (4), with a success rate of greater than 90% (5).
Nazar Golewale, M.D., founder and interventional radiologist with NG Vascular, says, “This procedure is a complete game-changer for patients suffering from chronic hemorrhoids. There is no hospital stay, no general anesthesia, no cutting, and no painful recovery. Just a couple of hours at our center and then the patient can return home and resume normal activities the next day. There will be noticeable improvement within the next 1-2 weeks.”
Dr. Golewale says that HAE can be performed again in the future if there is a recurrence, but he notes that this is a very rare occurrence.
“HAE carries a lower risk of bleeding, infections and other complications compared to surgery," Dr. Golewale adds. “Also, the risk of anal incontinence is a potential side effect of some surgical approaches, and that is completely avoided with HAE.”
HAE is recommended for those with chronic grade 1, 2 or 3 internal hemorrhoids and for whom conservative treatment has failed. For more information, or to schedule a consultation with Dr. Golewale, please call (219) 208-6218 or (708) 888-1167.
- About NG Vascular -
NG Vascular & Vein Center offers minimally invasive treatments for various conditions, from peripheral artery disease (PAD), knee osteoarthritis, uterine fibroids and several other conditions. With offices throughout Northwest Indiana & Chicago, the treatments are outpatient based, and patients benefit from greater convenience, a faster recovery and minimal discomfort. For information, please visit www.ngvascular.com.
References
1. Ganz RA. The evaluation and treatment of hemorrhoids: a guide for the gastroenterologist. Clin Gastroenterol Hepatol 2013; 11:593–603.
2. Nienhuijs SW, de Hingh IH. Pain after conventional versus Ligasure haemorrhoidectomy. A meta-analysis. Int J Surg 2010; 8:269–273.
3. Andreia Albuquerque Rubber band ligation of hemorrhoids: A guide for complications. World J Gastrointest Surg. 2016 Sep 27; 8(9): 614-620
4. Sandeep Bagla, MD et al. Outcomes of Hemorrhoidal Artery Embolization from a Multidisciplinary Outpatient Interventional Center. Journal of Vascular and Interventional Radiology. February 1, 2023.
5. Priscilla Mina Falsarella, MD et al. Embolization of the Superior Rectal Arteries versus Closed Hemorrhoidectomy (Ferguson Technique) in the Treatment of Hemorrhoidal Disease: A Randomized Clinical Trial. J Vasc Interv Radiol 2023; 34:736–744
Lew Pincus
NG Vascular & Vein Center
+1 (219) 208-6218
email us here
Visit us on social media:
LinkedIn
Instagram
Facebook
YouTube
X
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.